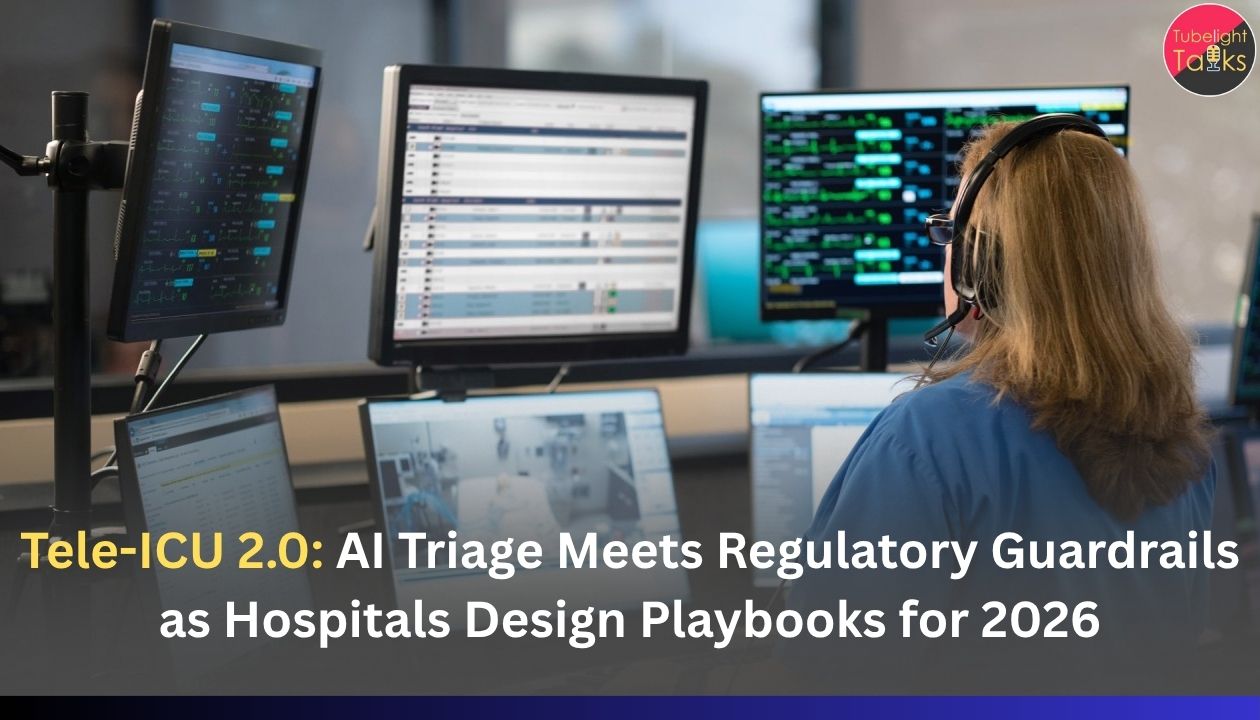
Tele-ICU 2.0: AI Triage Meets Regulatory Guardrails as Hospitals Design Playbooks for 2026
Tele-ICU has moved from pandemic stop-gap to mainstream critical-care strategy. Studies in 2023–25 show that tele-ICU “hub-and-spoke” models—where a central team of intensivists monitors multiple ICUs remotely—can be feasible and beneficial even in resource-limited settings, improving access to specialist care and standardising protocols.
At the same time, AI for triage and early warning in critical care—for sepsis, ARDS, cardiac arrest and general deterioration—is moving from papers to FDA-cleared tools and prospective pilots.
Layered on top is a fast-tightening regulatory net:
- The EU AI Act classifies most medical AI as high-risk, demanding strict risk management, data governance and human oversight, with key provisions kicking in between 2026 and 2027.
- The US FDA has updated guidance for AI-enabled device software and maintains an expanding public list of authorised AI/ML medical devices, including early-warning scores.
- India’s CDSCO has just released draft guidance on medical device software—explicitly covering AI and cloud-hosted tools—and is moving toward a four-class risk model for software as a medical device (SaMD).
Put together, these forces define Tele-ICU 2.0: AI-augmented remote ICU care, constrained by clear regulatory guardrails. Hospitals planning their 2026 roadmaps are now writing new playbooks that treat AI triage tools not as “smart gadgets” but as regulated, auditable components of critical care.
Tele-ICU 1.0: What we learned from the first wave
Early tele-ICU programs linked remote intensivists with bedside teams via audio-video, shared monitors and electronic records. Multiple evaluations have found:
- Benefits – better access to specialists, more consistent adherence to protocols, and potential reductions in ICU mortality and length of stay in some settings.
- Challenges – high upfront IT costs, unclear reimbursement models, resistance from bedside clinicians, concerns over data security, and variable impact on outcomes.
Crucially, Tele-ICU 1.0 was still human-led: remote teams watched monitors and EHRs, made calls, and advised bedside teams. AI tools, if used at all, were limited to basic rules-based alerts.
AI triage comes to the ICU
Between 2023 and 2025, AI in critical care has shifted from retrospective models to prospective early-warning and sepsis tools:
- Narrative reviews highlight AI’s role in real-time early warning systems for sepsis, ARDS, and cardiac arrest, often outperforming traditional scores when rigorously tested.
- The Prenosis Sepsis ImmunoScore became the first FDA-authorised AI tool for predicting sepsis risk within 24 hours of ICU admission, signalling regulators’ readiness to bring such tools into routine use.
- Other AI-enabled early-warning scores and risk monitors for deterioration are appearing on the FDA’s AI-enabled device list, even as the agency emphasises that such scores are medical devices requiring oversight, not casual decision aids.
Separately, AI research in emergency and virtual care triage (EDs, tele-emergency, and remote triage apps) shows potential to prioritise high-risk patients and reduce wait times, though many systems still face issues with fairness and external validation.
Tele-ICU 2.0 sits at the intersection:
AI models monitor streaming ICU data → trigger risk scores and alerts → remote ICU teams verify and act → bedside teams intervene.
That pipeline is exactly what regulators now want documented, validated and governed.
The new regulatory guardrails
1. United States: FDA lifecycle oversight for AI in Tele-ICU
The US FDA treats most AI triage and early-warning tools as Software as a Medical Device (SaMD) or as part of a device, subject to device regulations.
Key 2024–25 developments include:
- Draft guidance on “Artificial Intelligence-Enabled Device Software Functions: Lifecycle Management and Marketing Submission Recommendations” (January 2025), which emphasises post-market performance monitoring, change control plans and transparency about algorithm updates.
- An updated AI-Enabled Medical Device List (July 2025) showing rapid growth in cleared AI devices across imaging, cardiology and now early-warning scores and ICU monitoring.
For Tele-ICU programs using AI triage, US hospitals by 2026 will typically:
- Ensure tools are FDA-authorised for the intended use (e.g., sepsis prediction, deterioration alerts).
- Treat AI output as one input into clinician decision-making, with documented “human-in-the-loop” oversight.
- Maintain post-market surveillance logs—tracking performance, overrides, false positives/negatives and updates.
2. European Union: AI Act + medical device rules
The EU AI Act, effective from August 2024, categorises most medical AI as “high-risk”, especially when embedded in or as part of a regulated medical device. High-risk systems face requirements on:
- Risk management and incident reporting
- High-quality, representative training data
- Robust human oversight and transparency
- Post-market monitoring and conformity assessments
Some provisions for high-risk AI systems will apply around 2026–27, while guidance for general-purpose models with systemic risks is being phased in from 2025 onward.
For EU Tele-ICU networks, that means AI triage engines will need:
- Documented clinical performance in diverse ICU populations
- Clear descriptions of when and how clinicians can override an AI recommendation
- Integration into the existing Medical Device Regulation (MDR) framework for critical-care devices.
3. India and other emerging markets: Telemedicine rules meet SaMD
India’s Telemedicine Practice Guidelines (2020, updated commentary in 2022–25) already define norms for remote consultations: doctor identification, consent, data privacy and record-keeping.
What’s new for Tele-ICU 2.0 is software regulation:
- In October 2025, CDSCO issued a Draft Guidance on Medical Device Software, explicitly covering AI-enabled, cloud-hosted and network-based applications. It distinguishes SiMD (software in a device) from SaMD and proposes four risk classes (A–D) for software devices.
- The draft aims to align with global practice, making serious ICU-related AI tools likely Class C or D (moderate-to-high or high-risk), triggering stricter documentation, validation and quality management requirements.
For Indian hospitals, this implies that by 2026:
- Tele-ICU AI platforms used for triage, sepsis detection or deterioration warning will need to be treated as regulated medical devices, not just IT systems.
- Tele-ICU services must comply with both telemedicine guidelines (consent, confidentiality) and device rules (licensing, vigilance).
Hospital playbooks for 2026: What Tele-ICU 2.0 will look like
Hospitals preparing for Tele-ICU 2.0 are converging on a few practical playbook elements. Think of these as “operating system” choices for AI-enabled remote critical care.
1. Governance first: classify, approve, oversee
- Create an AI & Digital Health Oversight Committee (clinical, IT, legal, ethics, biomedical engineering).
- Maintain a registry of all AI tools touching ICU/tele-ICU workflows, with risk class, regulatory status and intended use.
- Require formal clinical and technical evaluation before deployment, including bias assessment across age, gender and comorbidities.
2. Human-in-the-loop, by design
- Define clearly who sees AI alerts first—bedside nurse, tele-ICU intensivist, or both—and within what time frame they must respond.
- Document when AI output is advisory versus when it triggers mandatory escalation (e.g., “red sepsis alert must be reviewed within 15 min by an ICU physician”).
- Build into the EHR/tele-ICU platform a simple way for clinicians to override and comment on AI suggestions, feeding back into quality and risk logs.
3. Tele-ICU workflow integration
Tele-ICU 2.0 workflows typically combine:
- Continuous streaming of vitals, labs and ventilator data into an AI risk engine.
- Tiered alerts (low, medium, high) pushed to tele-ICU dashboards and bedside teams.
- Protocolised responses: checklists for sepsis bundles, respiratory decompensation, or neurological change.
- Regular joint huddles between remote and bedside teams to review “top risk” patients flagged by AI.
Hospitals are writing standard operating procedures (SOPs) that specify exactly how Tele-ICU staff and ward teams react to each class of alert, to satisfy both patient-safety and regulatory expectations.
4. Data quality, logging and MLOps
- Ensure data pipelines (monitors, ventilators, lab systems, EHR) are reliable; many AI failures stem from missing or mis-mapped data rather than model logic.
- Maintain version logs of AI models and training datasets, as regulators increasingly expect traceability for performance drift or incidents.
- Implement routine performance audits—for example, quarterly reviews of sensitivity/specificity for sepsis alerts and false alarm rates, with changes discussed like M&M conferences.
5. Contracts, liability and reimbursement
- Vendor agreements increasingly include clear splitting of responsibilities (model quality vs. implementation vs. clinical use) and requirements for incident reporting.
- Hospitals and payers are testing tele-ICU reimbursement models that recognise AI-supported remote intensivist time, especially in “hub-and-spoke” networks and cross-border consults.
- Insurers and legal teams are asking for documentation of adherence to AI guardrails (EU AI Act, FDA guidance, CDSCO draft rules) as part of risk management.
6. Training and culture
- ICU nurses and residents need practical training on AI literacy: what the score means, when it can be wrong, and how to escalate.
- Tele-ICU 2.0 change-management focuses on avoiding both over-trust (“the AI said so”) and total scepticism, positioning AI as a second pair of eyes, not a replacement for clinical judgment.
Technology + Dharma in the ICU
From a Satgyan viewpoint, as emphasised by Sant Rampal Ji Maharaj, the true test of any technology—especially in life-and-death spaces like the ICU—is whether it aligns with Satya (truth), Nyay (justice) and Dayā (compassion), not just with financial or prestige metrics.
Applied to Tele-ICU 2.0:
- AI scores must be honestly represented—no over-claiming accuracy, no hiding limitations from clinicians or patients’ families.
- Hospitals have a moral duty to correct or withdraw tools that show dangerous bias or unreliability, not just because regulators demand it but because human lives are sacred.
- Tele-ICU plus AI triage can either deepen inequality (only elite hospitals get them) or extend high-quality critical care to rural and under-resourced hospitals through hub-and-spoke networks.
- A Dharmic approach prioritises deployments that reduce gaps—supporting district hospitals and small ICUs, not only high-margin private centres.
- Used well, AI can reduce alarm fatigue, catch deterioration earlier, and support staff in overwhelming situations—expressing compassion through better systems.
- But if deployed crudely, it can turn care into a series of impersonal alerts, widen fear of surveillance, and add stress to bedside teams.
Satgyan reminds us that no algorithm can substitute for the intention of seva (selfless service). Tele-ICU 2.0 will be truly successful only when AI is harnessed as a tool to serve patients equitably, transparently and kindly—within the guardrails of both regulation and Dharma.
Read Also: How AI Is Transforming Healthcare in India: A 2025 Revolution
FAQs: Tele-ICU 2.0
1. What is Tele-ICU 2.0?
It’s advanced tele-ICU combining remote intensivists with AI triage and early-warning tools, all operating under stricter medical-device regulations.
2. What AI tools are used in ICU triage today?
Sepsis predictors, early-warning deterioration scores, and real-time risk monitors for respiratory failure, cardiac arrest and organ dysfunction—supporting clinicians, not replacing them.
3. How do new regulations change Tele-ICU projects?
AI must be treated as a regulated medical device, with human oversight, monitoring, incident reporting, and strong data governance.
4. Can AI triage replace intensivists?
No. Current evidence and regulations support AI only as decision support, requiring human supervision for high-stakes ICU decisions.
5. What should hospitals do in 2025 for 2026?
Audit all AI tools, set up AI governance, pilot Tele-ICU 2.0 workflows, train staff, and align with FDA, EU AI Act or CDSCO rules.







Discussion (0)